Using CREATION Pinpoint®, the world’s only AI-powered and human verified global database of more than 3 million healthcare professionals’ social media profiles, Daniel Ghinn, Founder & CEO of CREATION.co reveals how social media and big data analysis is revolutionising our understanding of modern medicine.
Social media is transforming how we interpret and understand modern medicine. The growing use of platforms such as Twitter, Facebook and Reddit by healthcare professionals (HCPs) and their patients is creating a treasure trove of data. Parallel advancements in our capacity to analyse and interpret this information is offering real-world insights into drug and vaccine efficacy, side effects, interactions, as well as cutting-edge treatment options.
A demonstration of this can be seen in the shifting attitudes of HCPs towards the mixing and matching of different COVID-19 vaccines. Analysis of data from CREATION Pinpoint® the world’s only human verified and AI-powered global database of more than three million healthcare professionals’ social media profiles and their posts paints a vivid digital picture of how HCPs’ attitudes towards vaccine mixing has shifted over time and the key drivers behind these changes.
Chart 1 showcases this data. It shows a shift in attitudes among HCPs regarding the mixing of doses from being broadly negative or neutral at the start of 2021 to one of broad positivity as study data is published supporting the mixing of vaccines.

From January to April, HCPs mainly shared posts expressing distrust toward the mixing and matching of vaccines. They also shared reports from public health organisations, such as the FDA and Public Health England (PHE), not recommending the approach. Interestingly, while some HCPs shared the communication from PHE rejecting mix and match, other HCPs shared posts calling on the UK health authorities to allow for a mix and match regimen. This suggests there was some confusion at the time surrounding the topic due to a lack of clear data.
More from News
- The Fall Of Showering And The Rise Of Personal Hygiene Apps
- Have You Used The New Meta AI Feature On WhatsApp And Instagram?
- Experts Weigh In On Google Delaying Removal Of Third-Party Cookies Again
- Will TikTok Pull Out Of The US?
- UK’s Top 100 Fastest-Growing Female-Led Businesses Announced
- Will Robots Replace Warehouse Workers?
- UK Graduates Are Now Prioritising Higher-Paying Careers
- World Snooker Championships 2024: An Industry Of Winning Shots
Towards the middle of the year, HCPs began sharing data demonstrating the efficacy and safety of mixing COVID-19 vaccines, which in turn brought more clarity to the medical community and the public. One of the first major studies to be discussed was a study from Spain’s Carlos III Health Institute demonstrating that a first dose of AstraZeneca with a second dose of Pfizer is safe and effective.
Following the publication of the study’s findings a sharp rise can be seen in the numbers of HCPs being either positive or neutral towards the mixing of vaccines. In turn, some opinion leaders, such as Deena Hinshaw, Alberta’s Chief Medical Officer in Canada, began to advocate for the mixing of Pfizer and Moderna vaccines.
Pfizer on Top
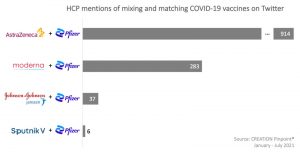
More detailed analysis of the data offers an important distinction. It shows that although HCPs discussed the effectiveness of mixing two vaccines, the majority advocated that the first dose could be from any number of approved vaccines, but that the second dose should be Pfizer. Of the first dose vaccines, AstraZeneca was the most mentioned by a significant margin.
Third Dose
With the booster rollout now underway in the UK and other jurisdictions, online discussions among HCPs have now shifted towards the efficacy of a third vaccine after either having a mix or two of the same vaccines. The prevailing opinion among experts is that a third dose will increase the immune response by increasing antibodies thereby decreasing COVID-19 cases globally. As this topic starts to emerge, and COVID-19 cases remain high, it is likely that mixing and matching vaccines will continue to be a topic of discussion for HCPs for the remainder of 2021.
Social Media And The Collation Of Real-World Evidence For Drug Safety Monitoring
The analysis above of the sentiments of HCPs towards COVID-19 vaccine mixing offers some insight into the role online analysis can play in improving our understanding of healthcare and pharmaceuticals. More broadly, the technique is demonstrating itself to have further reaching applications, ranging from the collation of real-world evidence for drug safety monitoring and efficacy to helping public health officials and pharmaceutical companies to better allocate resources to address emerging trends.



